In the intricate tapestry of human emotions and experiences, trauma stands out as a profound disruptor, capable of altering life in unforeseen ways. It’s a universal phenomenon affecting everyone across different walks of life.
The journey of understanding trauma is not just about recognizing its symptoms or tracing its origins but also about uncovering the resilience of the human spirit and pathways to healing, recovery, and realizing one’s full potential.
Defining Trauma
The American Psychological Association defines trauma as “the emotional response to a terrible event such as an accident, rape, or a natural disaster” (Rowell and Thomley, 2013). Trauma can manifest in people’s lives in various ways. It can appear as a single catastrophic event, such as the sudden loss of a loved one, or can be more challenging to detect in the form of pervasive verbal/emotional abuse (Start My Wellness, 2023).
Interestingly, not all individuals who experience trauma will go on to develop post-traumatic stress disorder. Many individuals will exhibit acute symptoms after exposure to trauma but never go on to develop chronic and systemic PTSD.
According to the National Institute of Mental Health, 6 out of 100 people will experience PTSD at some point in their lifetime (U.S. Department of Health and Human Services, 2023). Women are more likely than men to develop PTSD. Certain aspects of the trauma and personal genetic factors are also contributing factors as to whether or not an individual develops PTSD after being exposed.
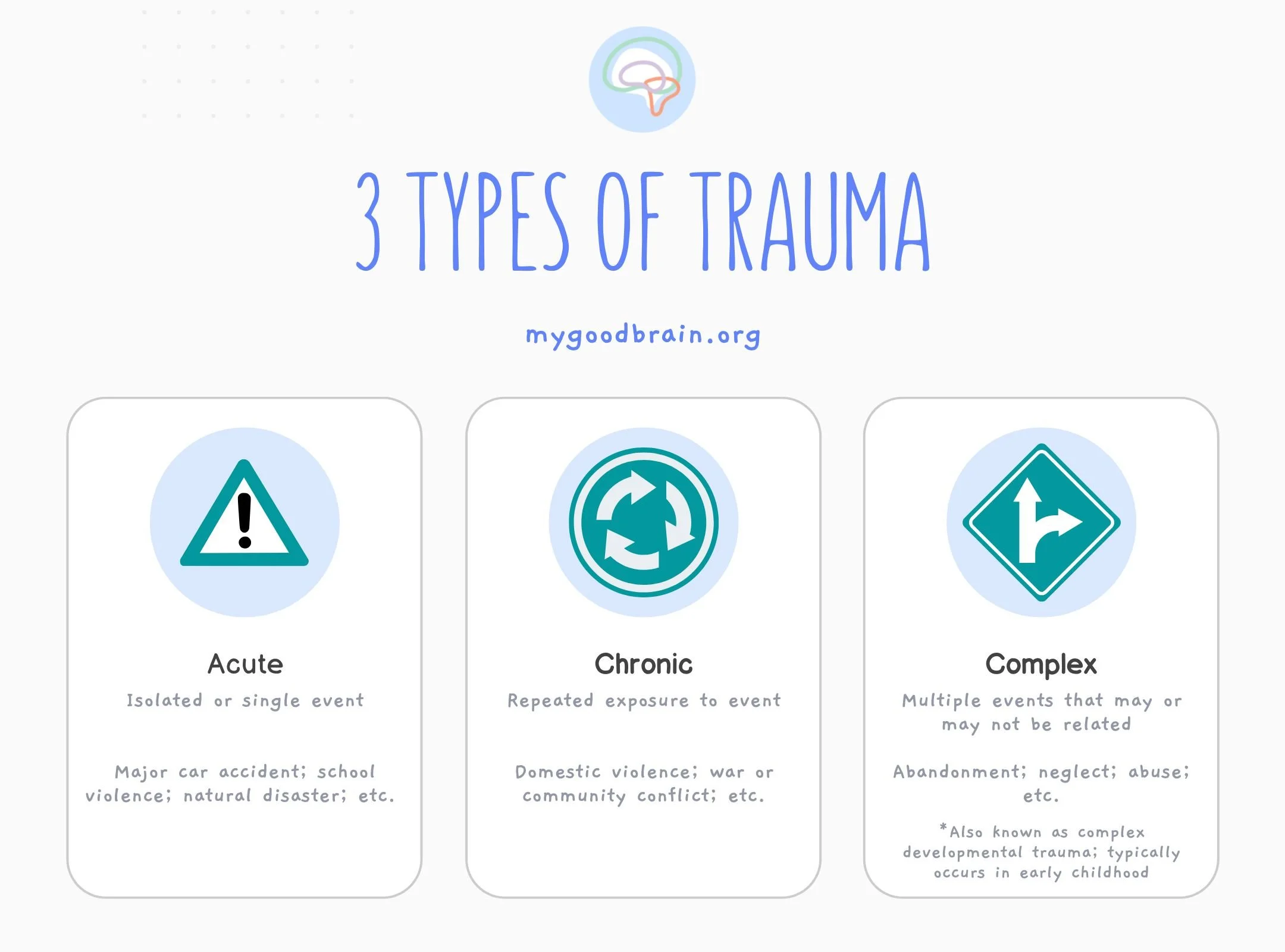
Picture Credit: MyGoodBrain
The Relationship Between PTSD and Trauma
Post-traumatic stress disorder (PTSD) has traditionally been associated with soldiers returning home from war-torn combat zones. Although well documented as a psychological condition throughout history, appearing in famous stories such as Shakespeare’s Henry IV, modern medicine did not start to officially recognize the impact of PTSD until World War I with the surge of soldiers suffering from “shell shock” (Crocq, 2000; Friedman, 2022).
It was then our communities started to realize the extensive nature of psychological distress caused by trauma. This realization thrust trauma into the forefront for investigation. However, there was still a significant delay in PTSD being understood as a severe and systemic issue.
It was not until the 1980s, more than 60 years after WWI ended, that the official diagnosis of Post Traumatic Stress Disorder was fully recognized by the medical community when it was added to the third edition of the Diagnostic and Statistical Manual of Mental Disorders. The impacts are far from fully understood. But there is indisputable evidence that trauma has a large effect on our brain, body, and mental state.
Picture Credit: Psychotherapy Central
Addressing Trauma: The Benefits of Trauma Informed Care
Now that our culture and community are starting to recognize the impact of trauma, there has been an outcry for treatment and support for those who have been exposed to traumatic events. Many organizations are starting to tout themselves as ‘trauma-informed,’ but what does that mean for you as a patient?
Trauma-informed care is not a type of treatment but rather an approach or philosophy of care (Start My Wellness, 2023). Implementing the approach can be challenging to measure and often varies from provider to provider. If your healthcare professional markets themselves as trauma-informed, it is crucial to understand this does not necessarily mean they have undergone any additional training or that they are utilizing an evidence-based approach for treating your trauma. Click here to read more about what it means to be trauma-informed.
When Do I Need to Seek Help for Trauma-Related Symptoms?
Trauma can cause a myriad of symptoms, which can have varying levels of impact on your daily life. It is important to seek help if the symptoms become uncomfortable, difficult for you to manage, and/or start to impact your work, relationships, or daily life.
Below are the common symptoms related to trauma exposure and the development of PTSD:
Picture Credit: Ample Mental Health
Symptoms can be more physical due to the chronic overactivation of the fight/flight system. These symptoms can appear in the body as:
- Muscle tension
- Difficulty with sleep
- Headaches
- Sweating
- Heart racing
- Dizziness
- Difficulty breathing
Mentally, a person can experience:
- Lower stress tolerance
- Inability to experience positive emotions
- Isolation
- Challenges connecting with others in relationships
PTSD often co-occurs and overlaps with another mental health diagnosis’ therefore, each person’s symptoms may differ or vary depending on their unique experience.
What are the Different Forms of Trauma Therapy?
No single modality for treatment is going to help you overcome trauma the same way. Your healthcare professional should assess your symptoms, the type of trauma you experienced, and how it is impacting your daily life to make an informed decision about what treatment may work best for you.
Picture Credit: Jocelyn Tsiah
The American Psychological Association has four trauma therapy types that are strongly recommended due to the level of research that supports their effectiveness. This includes: cognitive behavioral therapy, cognitive processing therapy, and prolonged exposure therapy (APA, 2020). An additional type of CBT has been created specifically for children and adolescents called Trauma Focused CBT (TF-CBT).
- Cognitive Processing Therapy – structured therapy which generally occurs over 12 sessions which includes psychoeducation, creation of a trauma impact statement, narration, and processing of traumatic event(s), and decreasing negative thought patterns related to the trauma (APA, 2017)
- Prolonged Exposure Therapy (PE) – utilized for patients with high avoidance of traumatic memories, feelings, or situations. This is done through gradual exposure to fear through imaginal and in-vivo (real-time) exposure to specific triggers (APA, 2020)
- Cognitive Therapy – focuses more on how the individual perceives the trauma and how thoughts related to trauma affect the patient’s current symptoms. The treatment works to adjust/change the pessimistic evaluation of the trauma to reduce the present feelings of threat (APA, 2017)
- Trauma-Focused CBT (TF-CBT) – created for use with children and adolescents. It is broken into three phases: stabilization, trauma narration and processing, and integration and consolidation. This treatment type generally involves both individual and family sessions. (Cohen and Mannarino, 2016).
In addition to these modalities, the American Psychological Association has three additional therapies and four medications that it conditionally recommends. These therapies have strong evidence that the treatment can lead to good outcomes. However, the evidence may not be as strong as those above.
- Eye Movement Desensitization & Reprocessing Therapy (EMDR) – this therapy aims to treat the neurobiological effects of trauma. Instead of focusing on the thoughts related to the trauma, this type of therapy directly targets the traumatic memories and how they are stored in the brain. The patient is guided to focus on the trauma while the healthcare professional stimulates both sides of the brain through the person’s senses (vision, touch, etc). (APA, 2017)
- Narrative Exposure Therapy (NET) – treatment modality is generally used in the group setting to treat trauma related to political, social, and cultural forces (i.e., refugee populations). Therapy occurs over 10 sessions in which individuals develop a whole life narrative and learn to reframe the life story to include, instead of revolve around, the personal trauma experienced (APA, 2017)
- Brief Eclectic Therapy (BEP) – combines techniques from cognitive behavioral therapy and a psychodynamic approach and is delivered over 16 sessions. The patient goes over the trauma verbally while the therapist assists the patient in dealing with distressing symptoms. The impact of the traumatic event is evaluated, and themes related to the event are identified. This type of therapy generally includes the creation of a relapse prevention plan (APA, 2017).
- Medications – Selective Serotonin Reuptake Inhibitors (SSRIs) are the gold standard for the treatment of PTSD. The Food and Drug Administration (FDA) has approved the use of the following SSRIs to help with symptoms related to PTSD: sertraline (Zoloft), paroxetine (Paxil), and fluoxetine (Prozac). The FDA has also approved the use of venlafaxine (Effexor) for PTSD, which targets both serotonin and norepinephrine pathways (APA, 2017). There are many other medications that providers may recommend for symptoms, but these are generally considered “off-label”. Some examples may include: Prazosin (Minipress) for nightmares, Propranolol (Inderall) for acute panic symptoms, and medications for insomnia such as trazodone (Deseryl) or mirtazapine (Remeron).
The most important thing to do if you feel as though you are experiencing the effects of trauma is to reach out for help. The first step can be scary and overwhelming, but you deserve peace and healing, so take the step.
Embracing Healing: Your Journey With Start My Wellness
Trauma and PTSD are not just conditions; they are experiences that profoundly shape lives, influencing every thought, interaction, and experience. The journey through trauma is deeply personal, with each individual facing their unique set of challenges and moments of resilience.
At Start My Wellness, we recognize the intricacies of trauma and the strength it takes to seek support. Our team of compassionate professionals offers a range of therapeutic services to provide a safe and understanding environment where your journey to healing is honored and supported every step of the way.
Call us at 248-514-4955 to get in touch and meet our therapists. Your journey to wellness starts here.

Author: Amy Fox, DNP
View Nurse Practitioner's Bio / Schedule Appointment
Looking for a Therapist? Start My Wellness has highly experienced Licensed Therapists that are currently accepting new patients.