In the past few years, the concept of neurodivergence has become more accepted as people understand that neurological differences are natural variations of the human brain’s vast potential. In the landscape of neurodiversity, a question often comes up: Is OCD neurodivergent?
Obsessive-Compulsive Disorder (OCD), a condition characterized by persistent unwanted thoughts (obsessions) and repetitive behaviors (compulsions), affects millions worldwide, influencing daily lives and mental well-being. OCD is a type of neurodivergence in that it leads to behavior and mental states that differ from the norm while significantly affecting everyday life and functioning.
In this article, we will cover what neurodivergence is, understand what OCD is, and evaluate ways in which OCD falls under the umbrella of neurodivergence while providing strategies and resources for those seeking treatment for OCD.
What is Neurodivergence?
Neurodivergence refers to any brain state (what the person feels) or neurological function (how the brain works) that diverges from what is considered typical by social standards and the majority of the population.
Neurodivergence is a concept that has significantly reshaped our understanding of mental differences between individuals. Originally coined within the Autism community in the 1990s, the term has since broadened to include a wide range of mental variations. This expansion includes conditions such as Autism, ADHD, Dyslexia, OCD, and others.
The term is also often used interchangeably with ‘neurodiversity,” and in most contexts, the two terms are meant to mean the same thing. For the purposes of this discussion, neurodivergence refers to brain chemistry and mental processes that differ from the ‘norm.’ Neurodiversity refers to the spectrum of cognitive processes that all individuals can experience. The neurodivergent spectrum refers to the umbrella of conditions that fall under neurodivergence.
In general, everybody is neurodiverse in that they can readily enter states of mental processing that may not be normal but are governed by context (whether environmental, social, chemical, etc.). Neurodivergent individuals experience these states as traits, consistently experiencing thoughts or behaviors that differ from the social norm.
However, the terms ‘normal,’ ‘abnormal,’ and ‘disorder’ carry a negative connotation, affecting how individuals see themselves and how peers and loved ones perceive them. In contrast, ‘neurodivergence’ and ‘neurodiversity’ allude to the differences we all share while acknowledging the inherent strengths of neurodivergent individuals.
Common Neurodivergent Conditions

Commonly recognized neurodivergent conditions each have their unique characteristics and challenges. Autism, for example, shows differences in social interaction and communication, while ADHD involves difficulties in attention and impulsivity.
Despite these challenges, it’s essential to acknowledge the strengths and individual differences within each neurodivergent condition, emphasizing the spectrum of diversity even within the same condition.
Commonly recognized neurodivergent conditions include:
- Autism Spectrum Disorder (ASD): ASD is characterized by differences in social situations and communication. Individuals with Autism may have specialized interests and proficient memory, creativity, and focus, giving them remarkable skills and perspectives.
- Attention Deficit Hyperactivity Disorder (ADHD): ADHD manifests as difficulties with attention, impulse, and hyperactivity. People with ADHD often struggle with organization and time management, but may also show high levels of creativity and spontaneity.
- Dyslexia: Primarily affecting reading and language processing, Dyslexia makes it challenging to interpret words, letters, and abstract symbols. However, these individuals often excel in spatial reasoning, creative thinking, and problem-solving.
- Tourette’s Syndrome (TS): Characterized by involuntary tics and vocalizations, Tourette’s Syndrome can be socially and educationally challenging. However, individuals with TS are often very creative, expressive, and good with improvisation.
Each of these conditions features a unique set of challenges and strengths, highlighting the neurodiversity of these conditions. While they differ in many ways, understanding the unique talents of neurodivergent individuals is essential for fostering inclusivity and understanding.
Common Symptoms of Neurodivergence
Neurodivergent conditions, while diverse in their characteristics, often share common symptoms. These shared symptoms can help identify and understand the range of neurodivergent experiences.
It’s important to note that the presence and intensity of these symptoms can vary significantly among individuals.
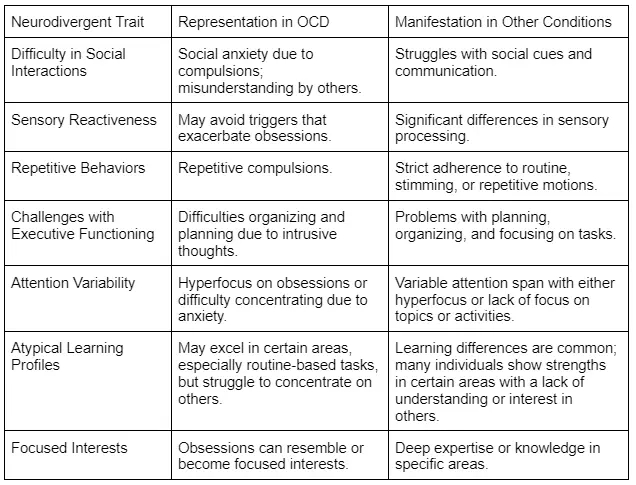
- Differences in Social Interactions: Many neurodivergent individuals experience social communication and interaction challenges. This can include difficulty reading social cues, making eye contact, or understanding sarcasm.
- Sensory Reactiveness: Heightened or reduced reactions to sensory input are common. This can include sensitivity to sounds, lights, textures, or tastes, which can be overwhelming or barely noticeable.
- Repetitive Behaviors: Engaging in repetitive behaviors or insisting on routines is common. These behaviors can provide comfort, structure, or a way to manage sensory overload.
- Challenges with Executive Functioning: Difficulties with executive functions, including planning, time management, and organization, are common.
- Attention Variability: Difficulty sustaining attention or, conversely, the ability to hyperfocus on specific interests is common in conditions like ADHD and ASD.
- Atypical Learning Profiles: Neurodivergent people frequently show learning differences. This may include exceptional abilities in certain areas and significant challenges in others.
- Focused Interests: Neurodivergent individuals develop deep, often highly specialized interests or skills. These can become a significant focus of their attention.
Understanding Obsessive-Compulsive Disorder

Obsessive-Compulsive Disorder is a complex mental health condition characterized by cycles of obsessions and compulsions. Obsessions are intrusive and unwanted thoughts, images, or urges that trigger distressing feelings. Compulsions are behaviors or mental acts an individual feels driven to perform in response to an obsession.
The obsessions and compulsions are never separate symptoms and work together in a cycle to create this complex condition. Obsessions, being unwanted and persistent, create anxiety and distress, which leads to compulsions. The compulsions are not enjoyable but rather a means to relieve the distress caused by pervasive obsessions.
The impact of OCD on daily life can be profound. The time and energy devoted to compulsive behaviors and the distress caused by obsessions can severely disrupt personal, social, and professional lives.
However, individuals who participate in therapy, particularly cognitive-behavioral therapy, can learn to better understand their condition, the underlying causes, and manage their symptoms.
What Are the Symptoms of OCD?
In addition to obsessions and compulsions, OCD can manifest emotional distress, anxiety, and daily functioning. Understanding these symptoms is essential for recognizing and appropriately responding to the onset of OCD.
- Obsessions: These are unwanted, intrusive thoughts, images, or urges that cause anxiety or distress. In most cases, individuals don’t want to follow through on these urges, but their persistent nature makes them very uncomfortable. Common obsessions include:
- Fear of contamination or germs.
- Worries about being harmed.
- Intrusive thoughts about shouting obscenities or acting inappropriately.
- Unwanted sexual or violent thoughts.
- Excessive concern with order, symmetry, or precision.
- Religious or moral obsessions.
- Compulsions: Compulsions are repetitive behaviors or mental acts that a person feels compelled to perform in response to an obsession. These are not enjoyable but rather provide order and stability to reduce stress. Common compulsions include:
- Excessive washing and cleaning to account for fear of contamination.
- Checking doors or locks repeatedly to alleviate fear of harm.
- Counting, tapping, repeating certain words, or doing routine behaviors to reduce anxiety.
- Ordering or arranging items in a particular way.
- Demanding reassurances or performing rituals to alleviate moral anxiety.
- Anxiety and Distress: In response to the cycle of obsessions and compulsions, individuals may become tense, anxious, or distressed; either due to the obsessions or from an inability to complete their compulsions.
- Avoidance: Individuals may avoid certain situations or environments that trigger their OCD.
- Impact on Functioning: OCD can impact many aspects of life, including work, school, and personal relationships, due to the time and energy spent on managing obsessions and compulsions.
What Causes OCD?
The causes of OCD are not fully understood, but research suggests they involve a combination of genetic, neurological, developmental, and environmental factors. These are considered risk factors in that they can increase the chance of OCD occurring, but no single factor causes OCD to develop.
Possible risk factors that may lead to OCD developing include:
- Genetic Factors: There is evidence to suggest a genetic component to OCD. Individuals with first-degree relatives who have OCD are at a higher risk of developing the disorder. However, the specific genes involved are not fully identified, and this remains a risk factor only.
- Neurological Factors: Brain imaging studies have shown differences in the prefrontal cortex and basal ganglia of individuals with OCD. These areas of the brain are involved in executive function and decision-making (prefrontal cortex), and physical responses to fear and anxiety (basal ganglia). However, other researchers note that these alterations may be symptomatic of, rather than a cause of, OCD.
- Developmental Factors: In some cases, OCD can develop from experiences during childhood, including attachment issues, trauma, and abuse, that create significant stress early in life.
- Environmental Factors: Certain environments can trigger or exacerbate OCD. These can include stressful life events and trauma at any life stage.
How OCD Overlaps with Neurodivergence
In the past, OCD has been traditionally categorized separately from neurodevelopmental conditions such as Autism or ADHD. However, as the concept of neurodivergence has evolved to include conditions that significantly impact daily functioning and mental states, many consider OCD to be a unique part of the neurodivergent spectrum.
This inclusion has to do with the overlap of symptoms neurodivergent conditions share with OCD, the rate at which OCD co-occurs with other conditions such as ASD, and the social recognition that individuals with OCD experience the world differently and have unique strengths and challenges.
Neurological features shared between OCD and other neurodivergent conditions are a key area of overlap. Research has indicated similarities in brain function and structure between OCD, Autism, and ADHD, especially in the development of the corpus callosum, the part of the brain responsible for communicating between both hemispheres.
Additionally, OCD shares many symptoms with other neurodivergent conditions, especially ritualistic behaviors, persistent thoughts, and social challenges. Cognitive rigidity, difficulty adapting to new situations or changing thought patterns, is a feature of both OCD and several neurodivergent conditions. This rigidity can manifest as persistent, intrusive thoughts or a preference for routine and predictability.
Social and communication challenges are another point of intersection. The time and mental energy devoted to managing OCD symptoms can significantly impact social interactions, mirroring the social communication difficulties that define many neurodivergent conditions.
Finally, the perspective of advocacy and representation is crucial. Including OCD in the neurodivergent spectrum allows individuals to benefit from advocacy and understanding that these conditions require, and to help foster the unique strengths and abilities of individuals with OCD.
Traits OCD Shares With Other Neurodivergent Conditions
OCD shares several traits with other neurodivergent conditions, highlighting its inclusion within the broader neurodivergent spectrum. Understanding these shared traits helps us understand the overlaps and unique challenges faced by individuals with OCD.
Differences Among OCD and Neurodivergent Conditions
While OCD shares traits with neurodivergent conditions, these overlaps also illuminate critical differences between these conditions, particularly in the context of how symptoms arise and are managed.
When examining social interactions, for instance, individuals with OCD may experience social anxiety stemming from their compulsive behaviors. This differs from the challenges faced by ASD or ADHD, where individuals have inherent difficulties understanding social cues or maintaining attention.
Ritualistic behaviors and routines are central to both OCD and conditions like ASD. However, in OCD, these behaviors are typically driven by anxiety and the need to alleviate distress caused by obsessions. In contrast, autistic individuals may engage in repetitive behaviors for comfort and predictability.
Additionally, executive functioning challenges present differently across conditions. OCD-related difficulties in organizing and planning are often a direct result of obsessions and compulsions. In ADHD, however, executive functioning challenges are more a pervasive aspect of the condition, often addressed with behavioral strategies.
These differences underscore the importance of personalized treatment plans that address the unique manifestations of each condition rather than applying broad strategies under the umbrella of neurodivergence.
The Importance of Tailored Therapy for OCD
The nuanced distinctions between OCD and other neurodivergent conditions indicate the importance of tailored therapy. With the appropriate therapist, treatment strategies can be intricately customized, taking into account the unique experiences and challenges of the individual.
Therapeutic approaches for OCD often center around Cognitive-Behavioral Therapy (CBT), particularly a specialized version known as Exposure and Response Prevention (ERP). This therapy is highly individualized, focusing on exposing the person to the source of their fear or obsession and helping them develop coping strategies.
In some cases, medication may be recommended alongside therapy to manage chemical imbalances (if present) to help individuals feel more comfortable and provide a better context for behavioral therapy.
Therapy for OCD may also include stress management techniques to promote relaxation. These techniques, including mindfulness and meditation, are tailored to help individuals with OCD navigate the intense emotions that accompany their condition.
Overall, OCD requires a nuanced, personalized approach to therapy. Personalized treatment plans that consider the individual’s specific symptoms, triggers, and life circumstances are vital so that individuals receive the most effective support possible.
Get Personalized Therapy and Empower Your Mental Health With Start My Wellness
OCD is a complex and nuanced condition that affects many individuals’ quality of life. It is a type of neurodivergent condition where an individual’s brain function and mental state are significantly affected by a cycle of obsessions and compulsions.
However, while OCD aligns with many neurodivergent conditions, its unique symptoms require personalized treatment. Recognizing OCD as part of the neurodivergent spectrum is not only about classification but also about tailoring therapy to embrace the strengths and address the challenges of those affected.
Start My Wellness understands the importance of individualized therapy. Our experienced therapists are equipped to assist individuals with any mental health condition, including OCD, with the compassion and expertise of years of experience navigating mental health.
Embrace your journey with Start My Wellness. Call us at 248-514-4955 or meet our therapists to begin your path to empowerment and better mental health.
Sources
- Harvard Health: What is Neurodiversity?
- Washington Edu: What do “Neurodiverse” and “Neurodivergent” Mean?
- National Library of Medicine: The Strengths and Abilities of Autistic People in the Workplace
- Healthline: The Benefits of ADHD
- Dyslexia Support: Strengths of Dyslexia
- Exceptional Individuals: Tourette’s Syndrome
- Exceptional Individuals: Neurodivergent Symptoms
- International OCD Foundation: About OCD
- Start My Wellness: Cognitive Behavioral Therapy
- National Institute of Mental Health: Obsessive-Compulsive Disorder
- National Library of Medicine: The Genetics of Obsessive-Compulsive Disorder: A Review
- National Library of Medicine: A Psychological and Neuroanatomical Model of OCD
- National Library of Medicine: The Neural Bases of OCD in Children and Adults
- Scientific American: Autism, OCD and Attention Deficit May Share Brain Markers
- Start My Wellness: ADHD and Relationships
- Start My Wellness: What is Rumination in OCD

Author: Anton Babushkin, PhD
Looking for a Therapist? Start My Wellness has highly experienced Licensed Therapists that are currently accepting new patients.